Wound closure techniques are essential for skin and soft tissue repair after trauma and surgery, and suture is still the most widely used closure method for all wound types. Ancient Egyptian literature describes them as far back as 3000 BC. In addition, archeologists have found sutures on mummies dating back to 1100 B.C. It is suggested that the original versions of suture threads were coarse and made from plants (linen, cotton, silk). The Greek physician Hippocrates recorded his use of sutures and plant-based materials, but the crude methods and materials most assuredly led to infections and severe scarring during that time of use.
Although the exact date of the transition from plant fibers to animal suturing materials is unknown, the first recorded use of catgut as a suturing material is attributed to Galen of Pergamon in the second century AD. Catgut was made up of twisted intestines of animals such as horses and sheep. Those materials were good choices since they were absorbable by body enzymes and provided good mechanical properties. But there was one crucial problem – surgical sutures often led to skin irritations and infections.

And only in 1860, Joseph Lister addressed the problem by creating a method for sterilizing suture material using carbolic acid. Chromic acid was later used to achieve sterilization, and then iodine was introduced to sterilize catgut in 1902. These substances significantly decreased the incidents of infection in sutured wounds. After that, eyeless needled sutures were invented. The thread was attached directly to the end of the needle.
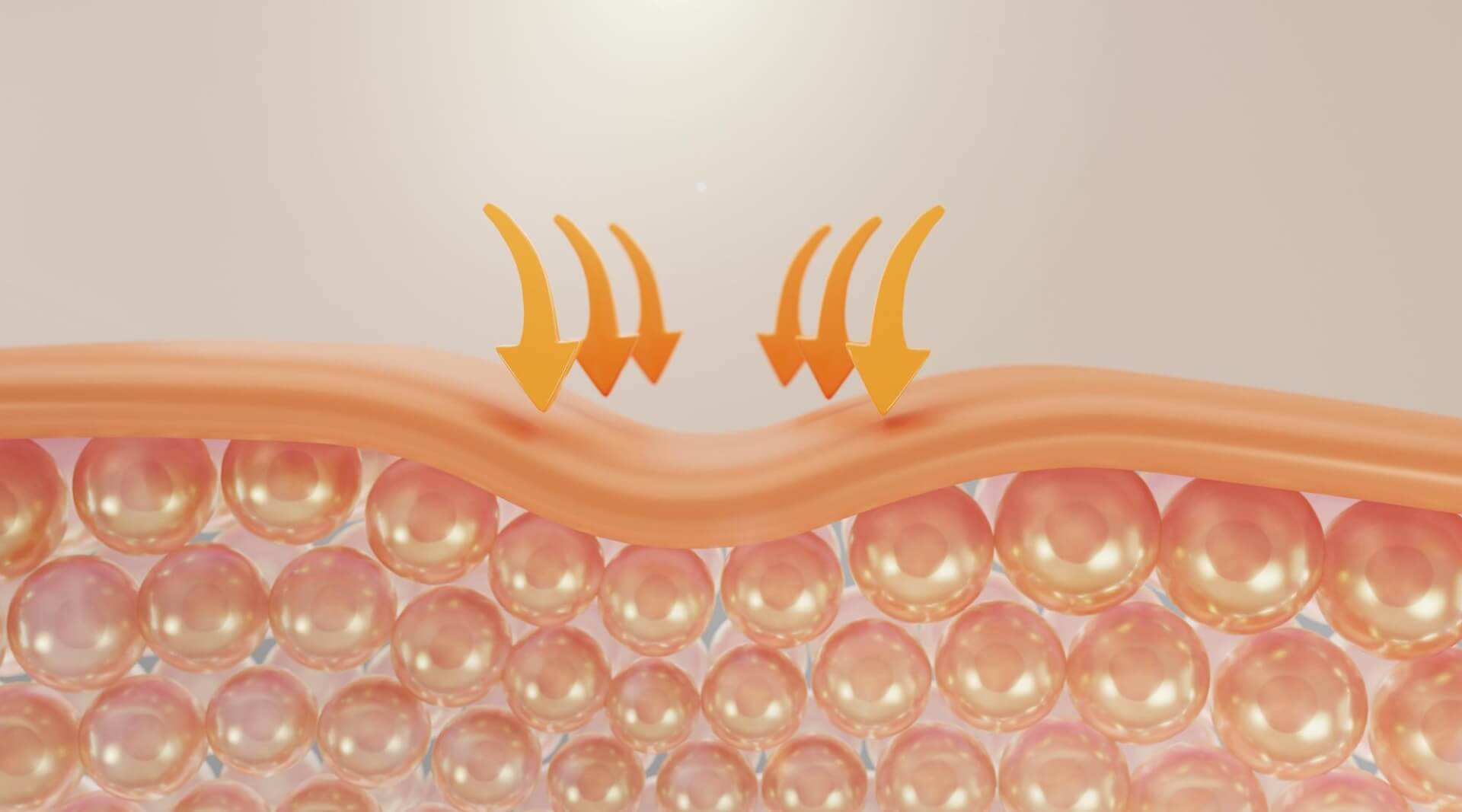
Suture techniques can be divided into percutaneous and subcuticular suture techniques. The subcuticular suture is an intradermal suture where the sutures are placed under the epidermis, in the dermis.
The origins of the subcuticular suture cannot be attributed to a single surgeon but rather a combined effort by generations of surgeons, beginning with Halsted in 1887. Halsted’s suture technique for skin closure over the repaired hernia cord involved burying interrupted fine silk sutures in dogs. These buried silk sutures were placed entirely within the lower layer of the skin without contacting contaminants on the skin surface. During the experiment, Halsted found that wound infection rates decreased notably with buried sutures. Gradually, the subcuticular suture has been proven to reduce the width of scars because of its tension-reducing effects on wound edges. Doctors have started using absorbable sutures instead of nonabsorbable sutures for subcuticular sutures.
The initial theory to close the wound with buried subcuticular sutures was to reduce the rate of infection, but later, in 1919, Davis advocated the role of the subcuticular suture more for aesthetic purposes and hence popularized its use. Further developments in the technique took place in the early 1960s when Straith proposed the introduction of an intradermal suture to reinforce, evert and decrease wound dehiscence, which subcuticular sutures cannot achieve.
Skin suturing promotes early wound healing, an essential process of scar formation. The permanent scar formed after wound healing can significantly affect patients’ mental health, personal relationships, and quality of life. The cosmetic effect can be poor if wound edges don’t contact accurately during the healing process.

The method of skin closure by subcuticular suturing is very popular amongst surgeons, especially plastic surgeons. This is because it gives better scarring than interrupted sutures, which may produce cross-hatching. Also, subcuticular sutures are usually absorbable, which prevents the need for suture removal, unnecessary pain, and inconvenience caused to the patient.
Appropriate application of subcuticular sutures can benefit patients, but they can still partially replace traditional ones. Compared with percutaneous sutures, the learning curve of the subcuticular sutures is longer, and intraoperative sutures take more time. Thin and fragile skin is unsuitable for subcuticular sutures, with risks of suture extrusion to the epidermal surface. Surgical sutures left in the skin may increase the risk of infection.
Currently, many suture methods, such as intradermal submerged sutures, intermittent submerged vertical mattress sutures, and wedge resection combined with improved submerged vertical mattress sutures, can partially achieve high cosmetic effects. However, wound tension should be minimized, and wound edges should be everted so that the germinating layers of the skin will be in contact with one another, and the optimal suture material should be chosen.

Download Free eBook “How much does Medical Animation explainer cost?”
- Should you choose Freelancer or Studio as a medical animation provider?
- What is the COST structure?
- Prepare BETTER for the project
- How to SAVE the budget?
- How to AVOID common mistakes?